The Colposcopy Clinic
This page has been produced to answer some of the commonly asked questions about your planned visit to the Colposcopy Clinic. You have been asked to attend the clinic for a colposcopy examination. This may be for a number of reasons. Your appointment letter will tell you exactly why you have been referred to us.
On this page
-
Why am I attending the Colposcopy Clinic?
-
Cervical cytology screening
-
What does an abnormal result mean?
-
Where is the cervix?
-
What is HPV?
-
Practical information before you attend your appointment
-
What is colposcopy?
-
Will I have to wait?
-
What happens before the examination?
-
What happens during the examination?
-
What if I have a biopsy?
-
What if I need treatment?
-
What can I expect after treatment?
-
Will the treatment affect my fertility?
-
What if I am pregnant?
-
Can I choose to delay treatment?
-
When will I get my results?
-
What do the results of the biopsy or treatment mean?
-
Will I need any follow up?
-
What if I have any questions?
-
Keeping to your appointment time
-
Students
-
Travelling after treatment
-
Contact information
-
Further information
Why am I attending the Colposcopy Clinic?
Abnormal cervical screening results is the most common reason for attending the Colposcopy Clinic, such as:
- HPV positive – borderline squamous/endocervical
- HPV positive – low grade dyskaryosis
- HPV positive – high grade (moderate or severe)
- HPV positive – possible glandular neoplasia of endocervical origin
- HPV positive – possible invasive cancer
- HPV Cytology Negative X 3
- Unavailable/unreliable HPV test
- HR HPV detected inadequate/insufficient cytology
In addition, you may be referred because:
- You have post–coital bleeding (bleeding after sexual intercourse)
- You have inter-menstrual bleeding (bleeding in between menstrual periods
- You have an unusual appearance of the cervix
Most people who have a colposcopy examination do not have cervical cancer.
Cervical cytology screening
The cervical cytology test that you had recently is a method of extracting cells from the cervix in order to look for evidence of High Risk HPV (HR HPV) that can cause cervical cell changes (abnormal cells) on the cervix. These cells, if left untreated, can develop into cancer.
HPV testing helps to identify who may be more at risk of developing cervical cell changes. If HR HPV is detected then the cervical cells will be examined and any abnormality will be graded to see if you need further investigations. Cervical screening is not a test for cancer.
Very few people with abnormal cervical screening have cancer as it usually takes an average of 12 to 15 years to develop. Regular cervical screening provides a high degree of protection against developing cervical cancer by detecting pre-cancerous changes.
The cervical screening programme saves the lives of 4,500 women, each year, in the United Kingdom. Not going for cervical screening is one of the biggest risk factors for developing cervical cancer. Colposcopy forms an integral part of the NHS Cervical Screening Programme and aims to reduce the number of women who develop cervical cancer and the number of women who die from it.
What does an abnormal result mean?
An abnormal result is very common, and usually means HR HPV has been detected and some abnormal cells have been found in the cells on your cervix. A change in cells is called dyskaryosis and acts as early warning signs that cancer of the cervix might develop in the future.
There are several grades of abnormality, your letter will specify your result (grade). It is important to remember that these changes are not cancer. They are pre-cancerous changes that if left untreated or unmonitored may develop into cancer.
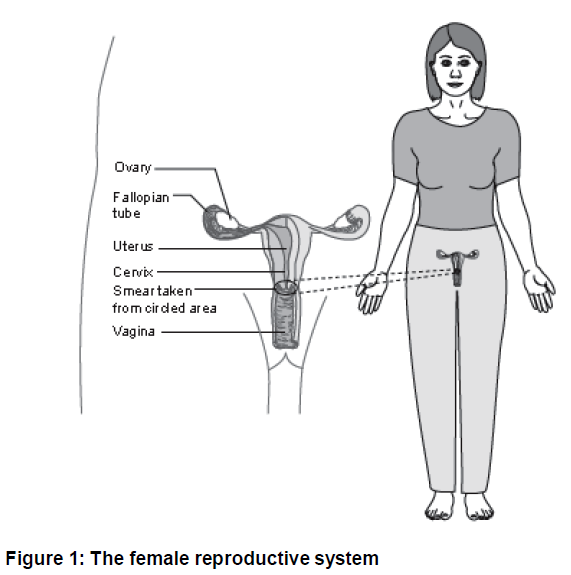
Where is the cervix?
The womb (uterus) is a pear-shaped organ situated at the upper end of the vagina. The cervix or neck of the womb is the narrow end of the pear shape, which projects into the upper end of the vagina. The cervix can be felt when a vaginal examination is performed and can be seen when an instrument (a speculum) is inserted in the vagina to hold the vaginal walls apart.
What is HPV?
Human Papilloma Virus (HPV) is a very common virus with over 100 different types that affect different parts of the body including the genitals. About 80% of the sexually active population will acquire the HPV virus at some point in their life. HPV is spread through close skin to skin contact during any type of sexual activity. Therefore, contact with HPV is considered to be a normal consequence of having sex. This is true whether heterosexual or in same sex relationships. There is no blame to attach to your current partner or any other partner or to yourself.
Most people are never aware they have been in contact with the virus as it usually clears on its own. The time between exposure to HPV and the development of cervical abnormalities is variable and HPV can remain dormant in some people for long periods of time without causing any problems or symptoms. This means an HPV infection may have come from a partner a long time ago.
In most cases the HPV will be cleared by the immune system and does not last long. But sometimes, HPV can persist in a small number of women and may lead to pre-cancerous cells on the cervix.
Having a family history of cervical cancer does not affect your chances of developing cervical cancer.
Smoking can affect the body’s immune system and make it harder for your body to get rid of the HPV virus. Please ask for a copy of the leaflet ‘GHPI0787 HPV information’.
Information about stopping smoking is available at www.nhs.uk/smokefree
Practical information before you attend your appointment
- If possible, avoid wearing thong type underwear as you may need to wear a sanitary pad after the examination.
- You are welcome to bring a friend or relative with you but it is advisable not to bring children.
- Please make sure that you have eaten breakfast or lunch before your appointment.
- If you have a coil (IUS/IUD) then this does not need to be removed as a colposcopy examination can still be performed.
- If you are pregnant, you can still have a colposcopy examination as this will not cause any harm to you or the baby.
- If you are taking anticoagulants (blood thinners), please contact the Colposcopy department on 0300 422 2914 for advice before the date of your appointment.
- It is fine to attend your appointment if you are on your period and experiencing light bleeding. If the bleeding is heavy or you would prefer to reschedule, please contact the Colposcopy department as soon as possible. If possible, please bring a sanitary pad with you.
- Bring a list of any medication you are currently taking.
What is colposcopy?
Colposcopy is a simple examination that allows a more detailed look at the cervix to examine the type and size of any abnormality. The instrument used in this examination is called a colposcope and is like a large magnifying glass which lets the doctor or nurse specialist look more closely at the changes on your cervix. The colposcope does not go inside you. All that goes inside you is the speculum, which is the same instrument used when a cervical cytology test is performed. For most women, this is a painless examination, but some may find it a little uncomfortable.
The examination takes about 15 minutes, but you will need to allow at least 1 hour for the whole visit.
Will I have to wait?
Your time is precious and we want to keep any waiting to a minimum. We try very hard to match your appointment time to our resources. Unfortunately, the clinic you are attending can involve personal and complex consultations. It is impossible to predict how long a consultation will take. This may mean that a consultation may run a long time over its allotted slot and as a result, means that the clinic overruns and a queue develops.
In addition, unexpected emergencies can pull doctors or nurses out of the clinic which can also lead to delays. We will try hard to avoid this as it can be frustrating for you. We will keep you informed of significant delays. However, we will make sure that you have all the time you need once your consultation begins. You will not be rushed.
What happens before the examination?
You will be seen by a colposcopy specialist who will take time to discuss your results before performing the examination.
You will be asked some questions about your periods, type of contraception you use, operations or illnesses you have had in the past and any medication you are currently taking.
The nurse will then show you to a changing room where you will be asked to undress from the waist down (you may not need to remove your skirt or socks).
What happens during the examination?
The nurse will help you to position yourself on a purpose-built couch which has padded supports for you to rest your legs on. When you are lying comfortably, the doctor or specialist nurse will gently insert a speculum into your vagina.
The examination will take longer than the smear test, about
15 minutes. This is because the colposcopist needs to have a careful look at the cervix using a colposcope and a number of different liquids which will be applied onto your cervix using cotton wool and cotton buds. The liquids will show up any abnormal areas and help the doctor or specialist nurse to see whether there are any abnormal changes present. This is not usually painful.
It is normal for photographs of the cervix to be taken during the examination. These will act as a record of the appointment and to provide a comparison at a follow up appointment if it is needed.
You can, if you wish, see your own cervix on a closed-circuit television screen attached to the colposcope. Tell the nurse in advance so she can set up the equipment.
The most common results are as follows:
Low grade changes
If the doctor or specialist nurse has identified some changes that appear low grade or are uncertain, a diagnostic biopsy is often needed to be sure of the diagnosis.
High grade changes
If the doctor or specialist nurse finds an area of abnormality suggesting high grade changes, this area will probably need to be removed. Providing you are agreeable; this procedure can often be done during your first visit. However, if you wish to delay treatment, then we would advise performing a small diagnostic biopsy and ask you to return on another day.
No abnormality detected
The doctor or specialist nurse may not find any abnormality. You would therefore be reassured and arrangements for follow up cervical cytology would be discussed.
What if I have a biopsy?
A tiny piece of tissue will be taken from the cervix for microscopic examination in the laboratory.
This should not be painful; however, you may feel a slight discomfort or stinging, which should not last long. After the biopsy, it is normal to have a discharge or light bleeding which can last a few days but no longer than 2 weeks. It is safe to use tampons during this time. It is best however not to have intercourse for up to 5 days, to allow time for the site where the biopsy was taken from to heal.
What if I need treatment?
Treatment can be offered at your first visit if your cervical cytology results showed high grade changes, which are then confirmed during the colposcopy examination.
The aim of the treatment is to remove the abnormal cells on your cervix. This will usually be done using a technique called LLETZ (Large Loop Excision of the Transformation Zone) and is normally performed under local anaesthetic. This may be offered to you at your first or following visit after the diagnostic biopsy. This procedure will take about 15 minutes.
Local anaesthetic is used to numb the cervix to make sure that you only feel minimal discomfort during the treatment. A small wire loop and an electrical current are used to remove the abnormal area and seal the wound at the same time. The tissue removed is then sent to the laboratory for further tests.
Occasionally, it may be better to treat while you are under general anaesthetic (asleep). If this is the case, the doctor or specialist nurse will explain the reasons for this decision in more detail.
It is very rare for hysterectomy to be considered; this is usually only the case if you have other gynaecological problems.
What can I expect after treatment?
You may have bleeding, similar to a period for the first week, followed by a blood-stained brownish discharge. This may continue for up to 3 weeks and can sometimes become watery and yellowish in colour. This is part of the natural healing process and varies from woman to woman.
Please remember to bring a sanitary pad with you to wear after your appointment. To make sure that the cervix heals as quickly as possible and to reduce the risk of infection, tampons, intercourse and swimming should be avoided for 4 weeks.
If the bleeding and discharge becomes excessive (not a period) or smells very unpleasant, and you have pain in your lower abdomen that does not get better with simple pain relief then please contact your GP for advice. You may need treatment with antibiotics.
Will the treatment affect my fertility?
This treatment should not affect your ability to become pregnant. However, some studies have suggested treatment may slightly weaken the cervix and can slightly increase the risk of premature delivery. Whereas other studies have shown that if you have ever had any pre-cancerous changes on the cervix, you are at a slightly higher risk of early labour than women who have not had these changes.
We therefore consider loop diathermy unlikely to have an effect on fertility or increase preterm labour. If you become pregnant after this treatment, we advise you to inform your GP and midwife that you have had loop diathermy treatment.
What if I am pregnant?
If you have just found out that you are pregnant, we still need to see you in the Colposcopy Clinic. A colposcopy examination is safe during pregnancy and should not affect the delivery of your baby. It is important that we see you in clinic to assess the changes on the cervix so that we can arrange the most appropriate follow up.
If you are pregnant, please do remember to tell the doctor or nurse just in case they are not aware.
If you need treatment this is usually performed 3 months after the delivery of your baby.
Can I choose to delay treatment?
If your cervical cytology test shows high grade changes, most women find it suitable to be treated at their first appointment. However, you may prefer to delay your treatment. For example, you might have a holiday planned in the days following your appointment and the bleeding after the treatment may be a nuisance for you.
There is no problem in delaying treatment for a short while. You will be sent a further appointment.
When will I get my results?
The results will not be available immediately as the tissue removed needs to be examined in the laboratory. It can take up to 4 weeks to receive the results by letter. This letter will explain the grade of abnormality detected and if anything further needs to be done.
What do the results of the biopsy or treatment mean?
The result of the tissue sample taken by biopsy or removed by LLETZ treatment are examined for the presence of precancerous changes, Cervical Intra-epithelial Neoplasia; more commonly referred to as CIN.
There are three grades of CIN 1, 2 or 3 depending on how many cells are involved.
CIN 1
These are relatively minor changes with a very low risk of progressing to cancer and will usually return to normal by themselves. Treatment is not usually necessary. You will require further cervical cytology tests at your GP’s surgery.
CIN 2, 3 and CGIN
These are more definite changes and, if you have not already had treatment at your first visit, you will normally be asked to come back to have the abnormal area removed.
Remember that you are very unlikely to have cancer. Only very rarely will a biopsy/LLETZ show cell changes that have already developed into cancer.
Will I need any follow up?
Everyone, who has had abnormal cervical screening, will continue to be followed up with cervical cytology tests when discharged from the Colposcopy Clinic.
If no abnormality was detected during the colposcopy examination or a cervical biopsy did not detect an abnormality, then you will return to routine cervical cytology tests every 3 or 5 years, depending on your age.
If CIN 1 was detected following your biopsy, then you will normally be discharged back to your GP for a cervical cytology test in 1 year.
If you have had treatment (LLETZ), then you will need to have a cervical cytology test in 6 months, usually with your GP. This sample will be tested to make sure that you have cleared the HPV that contributed to the initial abnormality (CIN).
Your doctor or specialist nurse will explain the required follow up in your result letter.
If you are discharged from the Colposcopy Clinic, the National Screening Services will send you notification when your next smear test is due. We advise you to keep a note of the date for your next screening test.
Treatment is almost always successful and it is unlikely that the CIN will recur. However, if further cervical cytology detects an abnormality or ongoing HR HPV then you will be referred back to the Colposcopy Clinic for a further examination.
What if I have any questions?
Most questions you may have can often be answered during your clinic appointment. However, if you have questions and would like an answer before your appointment, please do not hesitate to contact the Colposcopy Clinic.
Keeping to your appointment time
If you cannot attend your appointment for any reason, please let us know as soon as possible. This will allow us to offer it to another patient and rearrange your visit. Please be on time for your appointment; failure to do so is likely to result in a possibility that you will not be seen that day and will have to rebook. Although the examination only takes about 15 minutes, we ask you to allow at least an hour for the appointment.
Students
Students are the next generation of doctors and consultants and are working in the Colposcopy department to improve their knowledge. However, this does not mean that you need to have a student listening to your story. No one will examine you without your permission and no student will be involved without your consent. A student will not perform an internal examination unless you specifically consent to this. Do not feel under any pressure as no one will be offended if you prefer not have a student present during your consultation, examination or procedure.
Travelling after treatment
There is no medical reason to avoid travelling after treatment, but if you have any complications after the procedure while overseas, your insurance may not cover the medical attention you need.
Contact information
Colposcopy Helpline
Tel: 0300 422 2385
This is an answerphone service. Your call will be returned between Monday to Friday, 9:00am to 5:00pm
Email: ghn-tr.colposcopyhelpline@nhs.net
If you require urgent medical advice/assistance outside of these hours, please contact either your GP or NHS 111.
NHS 111
Tel: 111
Appointments
Tel: 0300 422 2914
Monday to Friday, 9:00am to 5:00pm
Further information
For more information, please visit the following website:
NHS Cervical Screening Programme
Website: www.cancerscreening.nhs.uk/cervical
Gloucestershire Domestic Abuse Support Service (GDASS)
This is a county-wide service offering a variety of support programmes for women and men over 16 years old who are experiencing domestic abuse.
Tel: 01452 726 570
Monday to Friday, 9:00am to 5:00pm
Domestic Violence Helpline
Tel: 0808 2000 247 (24 hours)
Email: support@gdass.org.uk
Website: www.gdass.org.uk