Having a trans-nasal endoscopy as an outpatient
You have been advised to have a trans-nasal endoscopy to help us to investigate the cause of your symptoms. This page contains information about having a transnasal endoscopy through the nose. It is important that you read this page before your appointment so that you understand about the procedure and the preparation involved.
If you have diabetes and you are receiving treatment, please leave a message on the Medication Advice Line. The number is at the end of this page. If you are using an insulin pump, we would like your BM to be 7mmol/L. Please call your local pump team if you need further advice.
If you are taking any medication that thins your blood other than aspirin (which you can continue to take), please contact the Medication Advice Line. This is very important as your procedure may be delayed if you do not get advice.
If you have broken your nose, had nasal surgery or have sinus concerns, please call the endoscopy unit you will be attending for your trans-nasal endoscopy. This may mean that the nasal route is not suitable for you.
What is a trans-nasal endoscopy?
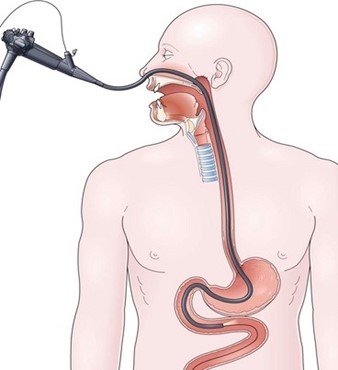
Gastroscopy is an investigation to look directly at the lining of the oesophagus (gullet/food tube), the stomach and around the first bend of the small intestine (the duodenum). A trans-nasal endoscope (scope) is passed through one of your nostrils down into the back of your throat, into the oesophagus, then stomach and duodenum.
A trans-nasal scope is a thin flexible tube, thinner than your little finger, and is a much smaller than a conventional gastroscope. It has a bright light at the end (this is not hot), which is necessary to be able to see the lining of the stomach.
Pictures are transmitted on to a screen so that any abnormalities can be seen.
Biopsy
A biopsy is a small sample of tissue that may be taken from the lining of your gut or bowel for further examination in the laboratory. It is taken using sterile biopsy forceps through the scope. This will not be painful.
Alternative procedures
The main alternative to a trans-nasal endoscopy is a barium meal X-ray. This can look at the stomach but does not allow biopsies to be taken. Please note that an alternative procedure will not be available on the day.
A barium swallow can capture X-ray images of the upper digestive tract, but it does not allow for direct visualisation.
Preparing for your procedure
To allow a clear view during the procedure the stomach must be completely empty. You are therefore asked not to have anything to eat for at least 6 hours before your appointment time. You may drink water up to 2 hours before your appointment time.
Admission to the department
On arrival at the department, you will be seen by a nurse who will check your personal details.
You will be asked a series of questions about any operations or illness that you may have had or are presently suffering with. Please bring a list of the medications you are currently taking.
The nurse will also ask if you have any allergies or have had any reactions to medicines or foods.
We are unable to provide sedation for this test, but please be assured that most people find TNE comfortable and well-tolerated without sedation. This is because the trans-nasal scopes are much smaller and are generally well tolerated by patients.
The test and possible complications will be explained so that you understand the procedure and any risks involved.
You will be asked to sign a consent form. By signing this form, you will have agreed to have the test performed and that you understand why it is needed. This does not take away your right to have the test stopped at any time.
For the time that you are in the department we want to provide a safe, supportive and pleasant environment. Please do not be afraid to ask if you have any worries or questions at this stage.
For this procedure you will not need to remove your clothes but ties may need to be loosened and shirts opened if they are tight at the neck.
Please remember that your appointment time is not the time you will have your procedure. There will be a wait between your admission and having your test done. A nurse will escort you into the room where the procedure will take place. The nurse will stay with you throughout the test. You will be made comfortable on a patient trolley, lying on your left side, with your knees slightly bent. This procedure can also be carried out with you in a sitting position. If you use a wheelchair, you can remain in your wheelchair to have the procedure carried out.
Anaesthetic nasal spray
Nasal anaesthetic spray is a local anaesthetic spray used to numb the nasal passages and the throat.
The nasal/throat spray has an effect very much like a dental injection and will reduce the feeling as the transnasal scope is passed through the nasal passage and throat during the test.
The benefit of having anaesthetic spray is that you are fully conscious (awake) and aware during the procedure. You are also able to talk while having this procedure done. You will be able to go home unaccompanied almost straight away after the procedure.
You will also be allowed to drive after discharge and carry on with your normal routine.
The restriction is that you must not have anything to eat or drink for 1 hour after the procedure.
This will allow for the sensation in your mouth and throat to return to normal.
It is strongly advised that your first drink after the procedure is cold. This should be sipped slowly to make sure that you do not choke.
You should avoid blowing your nose for 2 to 4 hours to prevent nosebleeds.
The procedure
In the examination room any dentures will be removed and local anaesthetic spray will be given via the nostrils and to the back of your throat to numb it for the procedure.
You will be able to talk throughout the procedure. The scope is inserted through either nostril. When it reaches the back of the throat you may be asked to swallow to help the tube go down into the stomach. This will not interfere with your breathing.
Some air will be passed through the scope to inflate your stomach and allow a clearer view. You may feel wind like discomfort and belch some air up during the test. This is normal so please do not be embarrassed.
Any saliva in your mouth will be removed using a small suction tube. When the scope is removed most of the remaining air in your stomach will also be removed. A trans-nasal endoscopy normally takes about 10 minutes.
Complications
Abdominal discomfort
It is common to feel bloated and have some wind associated pains due to the air that is used to inflate your stomach during the procedure. This should settle after a few hours.
Sore nose and throat
It is very common to have some nasal soreness and a sore throat. You will be asked not to blow your nose for 2 to 4 hours. If you blow your nose there may be a few spots of blood or you may have a small nose bleed.
If you had a biopsy taken you may cough or bring up a small amount of blood-stained fluid. This is normal and will pass within 24 to 48 hours.
When to seek advice
If you experience any of the symptoms listed below, please contact the Endoscopy Unit where you were seen, for advice:
- Abdominal pain / severe tenderness (not caused by wind).
- A firm or swollen abdomen.
- High temperature.
- Vomiting.
- A persisting and worsening nose-bleed that will not stop.
- You pass blood red or black bowel movements.
After the procedure
After the trans-nasal endoscopy is completed, the nurse caring for you during your test will take you from the endoscopy room to the recovery area.
Normally you do not see the person who performed your procedure before going home.
Your nurse will go through the report with you and provide you with an after-care leaflet before you are discharged.
If a sample (biopsy) has been taken, the result can take up to 5 weeks to process. You may be given an outpatient’s appointment to return for review.
Alternatively, the results will be forwarded to your GP and you will need to make an appointment to see him/her. A report of the procedure will automatically be sent to your GP.
Contact information
Appointment Enquiries Cheltenham General Hospital
Tel: 0300 422 6899
Monday to Friday, 8:30am to 4:00pm
Gloucestershire Royal Hospital
Tel: 0300 422 6351
Monday to Friday, 8:30am to 4:00pm
Medication Advice Line (Answer Machine)
If you have any questions relating to your medication, please leave a message. A member of staff will return your call normally within 24 hours, week days only.
Cheltenham General Hospital
Tel: 0300 422 3370
Monday to Friday, 8:00am to 6:00pm
Cirencester Hospital
Tel: 0300 421 6294
Monday to Friday, 8:00am to 4:00pm