Having a gastroscopy as an inpatient
You have been advised to have a gastroscopy, which you may also have heard being called an endoscopy or OGD (meaning an oesophageal-gastro-duodenoscopy). A gastroscopy will help us to investigate the cause of your symptoms. It is important that you read this page before your appointment so that you understand what will happen during this procedure and the preparation involved.
What is a gastroscopy?
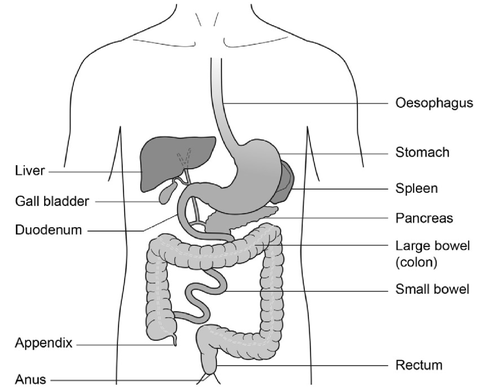
Gastroscopy is an investigation to look directly at the lining of the oesophagus (gullet/food tube), the stomach and around the first bend of the small intestine (the duodenum). A gastroscope is passed through the mouth, down the gullet and into the oesophagus. A biopsy, if required, can be taken during this procedure.
A gastroscope is a long flexible tube, thinner than your little finger. It has a bright light at the end (this is not hot), which is necessary to be able to see the lining of the stomach.
Pictures are transmitted on to a screen where any abnormalities can be seen.
Biopsy
A biopsy is a small sample of tissue that may be taken from the lining of your gut or bowel for further examination in the laboratory. It is taken using sterile biopsy forceps through the scope. This will not be painful.
The following treatments can be performed via the endoscope. This would be discussed with you by the Endoscopist before the gastroscopy is performed. Any risks associated with these treatments will also be explained to you.
Banding
Banding is a way to treat oesophageal varices. These are like varicose veins in your oesophagus. The endoscopist will place special elastic bands around each of the varices. This stops the blood supply to these veins and they eventually disappear. This will not affect the normal blood supply to the oesophagus.
Dilatation
A dilatation can be performed if a narrowing of the gullet (oesophagus) is found. This means stretching the narrowing to improve your swallowing.
Stenting
An oesophageal stent is an expandable tube made of a flexible metal which allows it to expand over a period of hours. This will make it easier for you to swallow food and fluids. Your consultant will choose the right stent and size for your needs. This procedure is carried out under X-ray to make sure that the stent is placed correctly.
Preparing for your procedure
The test and possible complications will be explained so that you understand the procedure and any risks involved.
You will be asked to sign a consent form by the ward doctor. By signing the consent form, you will have agreed to have the test performed and that you understand why it is needed. This does not take away your right to have the test stopped at any time.
To allow a clear view during the procedure the stomach must be completely empty. You are therefore asked not to have anything to eat for at least 6 hours before your appointment time.
You may have sips of water up to 2 hours before your appointment time.
You will be offered a choice of sedation and/or throat spray.
On arrival at the Endoscopy Unit
You will be seen by a nurse who will check your paper work details and record your observations. The nurse will also ask if you have any allergies or reactions to medicines or foods.
You might also be given a small dose of Infacol®, by mouth, to reduce the secretions in your oesophagus and bowel. It will also give a better view of your oesophagus and stomach during the procedure. Please do not have any other liquids after you have been given the Infacol® - the nurse giving you this medication will also remind you not to have any further fluids.
You will be asked if you want sedation.
A nurse will take you into the room where your procedure will take place. Depending on how you have travelled to the Endoscopy Unit, you will either be on your hospital bed or one of the Endoscopy trolleys. A nurse will stay with you throughout the test. You will be made comfortable lying on your left side, with your knees slightly bent.
Anaesthetic throat spray
Throat spray is a local anaesthetic spray used to numb the throat. This can be given on its own or alongside sedation.
The throat spray has an effect very much like a dental injection.
You must not have anything to eat or drink for about 30 minutes after the procedure. This will allow for the sensation in your mouth and throat to return to normal. It is strongly advised that your first drink after the procedure should be cold. This should be sipped slowly to make sure that you do not choke.
Intravenous sedation
Sedation will be given into a vein in your hand or arm. This will make you feel lightly drowsy and relaxed but not unconscious (asleep). You will be in a state called conscious sedation. This means that, although drowsy, you will still hear what is said to you and therefore will be able to follow simple instructions during the procedure. You will be able to breathe normally throughout the procedure.
The procedure
In the examination room any dentures will be removed and a local anaesthetic spray will be applied to the back of your throat to numb it for the procedure.
To protect your teeth and the gastroscope, a plastic mouth piece will be put between your teeth or gums if dentures have been removed. The tube will then be inserted through the mouth piece. When it reaches the back of the throat you may be asked to swallow to help the tube go down into the stomach. This will not interfere with your breathing.
Some air will be passed through the instrument to inflate the stomach and allow a clearer view. You may feel wind like discomfort and belch some air up during the test. Please do not be embarrassed.
Any saliva in your mouth will be removed using a small suction tube. When the gastroscope is taken out most of the remaining air in the stomach will also be removed. A gastroscopy normally takes 5 to 15 minutes.
Complications
Sedation can occasionally cause problems with breathing, heart rate and blood pressure. If any of these problems occur, they are normally short lived. Minor complications with sedation happen less than 1 in every 200 examinations.
A few people are excessively sensitive to the sedation we use and become too sleepy. This effect can be rapidly reversed with medication.
Major complications with endoscopies are very rare (less than 3 in 10,000) and death arising from these is extremely rare (less than 1 in 30,000).
The main serious complication is perforation (a tear) of the oesophagus (gullet) or bowel, which may need an operation. This complication is more common if a stretch is performed for narrowing of the gullet (less than 1 in 200). It would not be normal practice to stretch the gullet without discussing the risks and benefits with you first. If banding is performed, in less than 1 in 100 cases bleeding can be started.