Having a colonoscopy and polyp removal as an outpatient
You need to have a further colonoscopy to attempt to remove the polyp(s) found at the time of your last procedure. It is important that you read this information before your appointment so that you understand this procedure and the preparation involved.
If you currently take medicines containing iron, you must stop taking them 7 days before your appointment. The procedure may be delayed if you have not stopped taking the iron medicine.
If you have diabetes or are taking any medication that thins your blood, other than aspirin (which you can remain on) please contact the relevant Endoscopy Unit on the Medication Advice Line (answer phone). The telephone numbers are at the end of this page.
If you are an insulin pump patient, we would like your BM to be 7mmol/L. Please call your local pump team if you need further advice.
What is a colonoscopy?
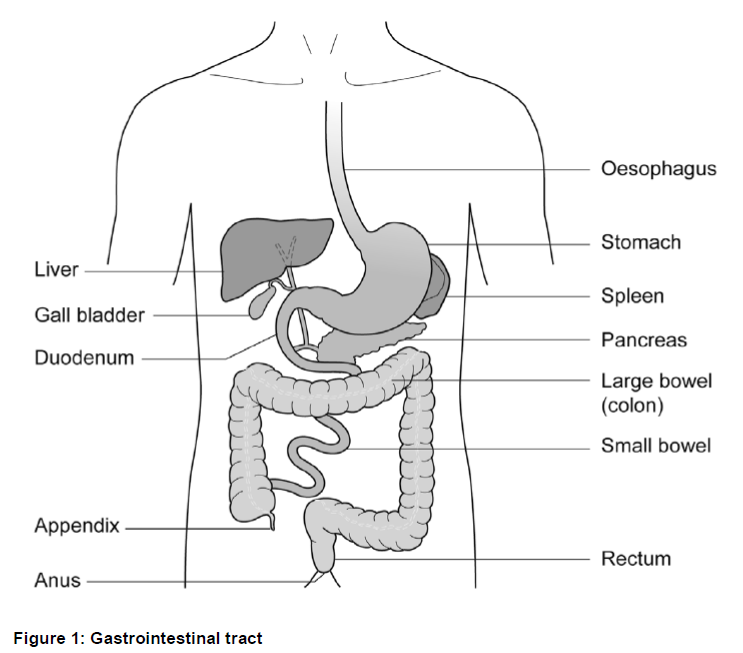
Colonoscopy is an investigation to look directly at the lining of the large bowel (colon) and also allows the opportunity to perform therapy such as removing polyps. In order to do this, a colonoscope is passed through the anus (back passage) and into the bowel.
The procedure is likely to be a little longer than the standard colonoscopy time slot. This is to allow sufficient time to remove the polyp(s) completely and deal with any complications that may arise. You can expect to be in the theatre for around 2 hours. The actual time taken may be more or less than this. It is possible that you may be in the department between 3 to 7 hours.
Polyps
It is possible to remove polyps during a colonoscopy using a special snare. This procedure should not be painful. Polyps are abnormal bits of tissue, like warts, which after removal, are collected and sent to the laboratory for further examination. It may take several weeks before the final report is available.
Alternative procedures
The main alternatives to colonoscopy removal of polyps are do nothing (with a risk of the polyp becoming malignant (cancerous) or to have the section of bowel containing the polyp removed by conventional surgery requiring a general anaesthetic. There is evidence that colonoscopic removal of the polyps is the best and safest approach.
Preparation for your procedure
To allow a clear view during the procedure the bowel must be cleaned using a special preparation.
You should have received your bowel preparation and full instructions on how to take it. The instructions will also include what you can eat and drink before the colonoscopy.
If you have not received the preparation, or have any questions about it please telephone the Medication Advice Line. The telephone number is at the end of this page.
Please note that you can drink clear fluids while taking the preparation right up to until your appointment time.
Clear fluids can be black tea or coffee, Bovril® or Oxo®, any squash except blackcurrant as it stains the bowel, apple juice or any other juice as long as it does not contain bits.
The NHS, a major contributor of carbon emissions in the UK, has recently outlined ambitious targets to achieve net zero carbon emissions by 2040. The endoscopy team in Gloucestershire have carefully considered ways of adopting more sustainable care and waste reduction.
We would appreciate your support to help make our practice ‘greener’ by kindly bringing the following items along to your endoscopy appointment, so that single use alternatives are not required:
- Dressing gown
- Pair of slippers
- Clean underwear to change into after the procedure
- If applicable, your own denture pot, hearing aid case(s) and/or eye glasses case
- Water bottle
- Reusable cup with lid for a complimentary hot drink after the procedure
- Bag to place your clothes in during procedure
On admission
On arrival at the department, you will be seen by a nurse who will check your personal details.
You will be asked a series of questions about any operations or illness that you may have had or are presently suffering with. Please bring a list of all medications you are currently taking.
The nurse will also ask if you have any allergies or reactions to medicines or foods.
You will be asked if you want sedation. If you are considering sedation, you will be asked to confirm that you have a responsible adult to take you home when you are ready for discharge. You must also have a responsible adult with you at home for 24 hours following the procedure.
The test and possible complications will be explained so that you understand the procedure and any risks involved.
You will then be asked to sign a consent form. By signing this form, you will have agreed to have the test performed and that you understand why it is needed. This does not take away your right to have the test stopped at any time.
Next you will be asked to change into a hospital gown. If you are attending your appointment at Gloucestershire Royal Hospital you can bring a dressing gown and slippers with you.
Please remember that your appointment time is not the time you will have your colonoscopy. There will be a waiting time between your admission and having your test done.
For the time that you are in the department we want to provide a safe, supportive and pleasant environment so please do not be afraid to ask if you have any worries or questions at this stage.
The colonoscopy
A nurse or doctor will escort you into the room where your colonoscopy will take place. A nurse will stay with you throughout the test. You will be made comfortable on a couch, lying on your left side, with your knees slightly bent. It is usual for patients to be asked to move several times during the procedure (back, both sides and sometimes face down) to help insert the colonoscope and enable the removal of the polyps.
Intravenous sedation
The sedation will be given into a vein in your hand or arm. This will make you lightly drowsy and relaxed but not unconscious. You will be in a state called conscious sedation. This means that, although drowsy, you will still hear what is said to you and therefore will be able to follow simple instructions during the investigation. Sedation also makes it unlikely that you will remember anything about the procedure. You will be able to breathe normally during the procedure.
For procedures involving polypectomy, due to the longer duration of these procedures, we advise patients to have sedation.
While you are sedated, we will check your breathing and heart rate so that any changes will be recorded and dealt with accordingly. For this reason, you will be connected by a finger probe to a pulse oximeter which measures your oxygen levels and heart rate during the procedure. Your blood pressure will also be recorded.
Please note that if you decide to have sedation you should not drive, drink alcohol, operate heavy machinery or sign any legally binding documents for 24 hours following the procedure. You will need someone to accompany you home and stay with you for 24 hours.
If suitable, Entonox® (gas and air) is also available during the procedure either as an alternative to sedation or as well as. This will help to control any discomfort. You will not need a responsible adult to stay with you if you choose Entonox® only. (A separate leaflet has been provided).
If you have experienced or suffered with any of the following within the last 12 weeks, Enotonx® will not be suitable for you.
- Pneumothorax
- Air embolism
- Emphysema/COPD
- Recent ear/eye surgery
- Head injury with impaired consciousness
- Bowel obstruction
- Scuba diving
- Decompression sickness
You will be in the department between 3 to 7 hours. The time taken for the removal of the polyp will depend on many factors. Generally, patients are admitted by 12:00 noon but could be in the unit until 6.00 pm or longer depending on the polyp removal and recovery.
Risks associated with having sedation
Sedation can sometimes cause problems with breathing, heart rate and blood pressure. If any of these problems happen, they are normally short lived.
Careful monitoring by a fully trained endoscopy nurse makes sure that any problems are identified and treated rapidly.
Older patients and those who have health problems, for example, people with breathing difficulties due to a chest problem will be assessed by a doctor before the procedure.
Complications
Complications are uncommon with diagnostic (investigative) procedures and are mostly due to the sedation given. Major complications are very rare. Complications are more common with therapeutic procedures such as polypectomy.
It is important to understand that any complications that arise during the procedure are normally dealt with by the endoscopist at the time they happen.
Bleeding is very common during a polyp removal and almost considered to be a normal part of the procedure, but it is very rare for it not to be controlled. Bleeding can happen up to 14 days after the procedure. A small amount of fresh red or altered blood is common and happens to 5 to 7 people out of every 100. This normally settles without any need for further intervention. One in every 150 people may need a blood transfusion if the bleeding continues.
Very rarely the colonoscope can cause damage to the bowel wall which can lead to a hole know as a perforation. This happens in less than 1 in every 1000 cases and is normally treated at the time of the procedure without further complications. If there are any concerns, you will be admitted to the hospital overnight, or longer, for antibiotic treatment.
As the procedure is a little longer, some patients can experience bloating, nausea or vomiting as a result of gas distending the bowel. This normally settles within a few hours if it happens.
The overall chance of missing something important such as a cancer is less than 1 in every 2,500 patients.
After the test
After the colonoscopy is completed, the nurse caring for you during your test will take you from the endoscopy room to the recovery area.
Your pulse and blood pressure will be monitored as needed. This is called the recovery period.
You may feel a little bloated or have some discomfort in your lower abdomen after the test. This is normal and it should start to ease by the time you are discharged.
You will need to stay in hospital for about 1 hour after the procedure depending on how you recover from the sedation given.
Normally you will see the person who performed your procedure before going home. Occasionally, this is not possible and our nurse will tell you the results of the test before discharge.
If you have had sedation, it is a good idea to have someone with you at this discussion as many people find they forget what has been said to them. You will be given written information to take home.
If a sample (biopsy or polyp) has been taken, the result will take up to 5 weeks to process. A report of the procedure will automatically be sent to your GP.
Normally after a larger polyp resection, the endoscopist will arrange a telephone follow-up consultation.
Going home
If you have had sedation, it is essential that someone takes you home and that there is a responsible adult to stay with you for 24 hours.
You may go home by taxi or public transport but you must have someone to accompany you on the journey.
For this period of time, you should not:
- Drive a car, motorbike or ride a bicycle
- Drink alcohol
- Operate machinery or do anything requiring skill or judgment
- Make important decisions or sign any documents
If you did not have sedation the above paragraph does not apply.
An advice sheet including this information will be given to you before you leave; this is your discharge letter. You will be given a procedure report. A copy of the report will also be sent to your GP.
If you have a polypectomy (polyp removed from your bowel) there is a risk of delayed bleeding. If the polyp is large or there are lots to be taken away it is important to let your endoscopist know if you intend to travel (especially long haul flights) in the days following this treatment.
Gloucestershire Hospitals NHS Foundation Trust is an Endoscopy Training Centre. We regularly have registrars and nurse endoscopists working on the unit. Please discuss any concerns or issues you may have with the admission nurse.
Results
Please contact your GP or consultant directly for your test results as these are not disclosed to Endoscopy.
Contact information
Appointment enquiries
Tel: 0300 422 6350
Tel: 0300 422 6351
Monday to Sunday, 8:30am to 4:00pm
Medication Advice Line (answer machine)
If you have any questions relating to your medication, please leave a message and a member of staff will return your call:
Cheltenham General Hospital
Tel: 0300 422 3370
Monday to Friday, 8:00am to 6:00pm
Gloucestershire Royal Hospital
Tel: 0300 422 8232
Monday to Friday, 8:00am to 6:00pm
Saturday and Sunday, 9:00am to12:00 midday
Other Endoscopy Units
Cirencester Hospital
Tel: 0300 421 6294
Monday to Friday, 8:00am to 4:00pm
Stroud General Hospital
Tel: 0300 421 8073
Monday to Friday, 8:00am to 6:00pm