Cystoscopy and urethroscopy
This page gives you information about having cystoscopy and/or urethroscopy.
On this page
-
What is cystoscopy?
-
What is urethroscopy?
-
Why do I need a cystoscopy and/or a urethroscopy?
-
What is a flexible cystoscopy?
-
What is a rigid cystoscopy or urethroscopy?
-
What is a check cystoscopy?
-
Alternative investigations
-
Possible risks
-
Pre-assessment
-
Before the operation
-
Discharge
-
Contact information
What is cystoscopy?
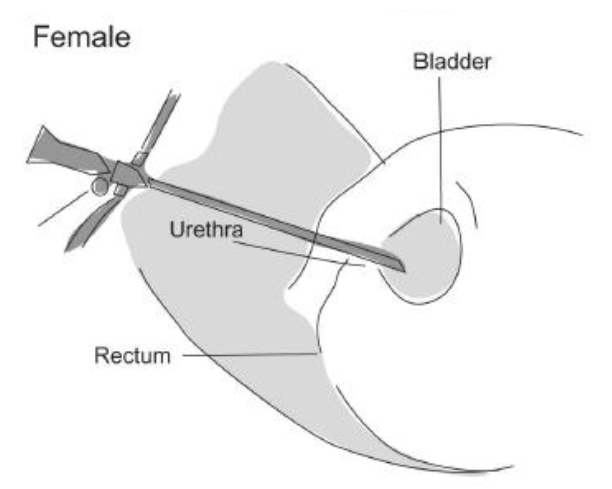
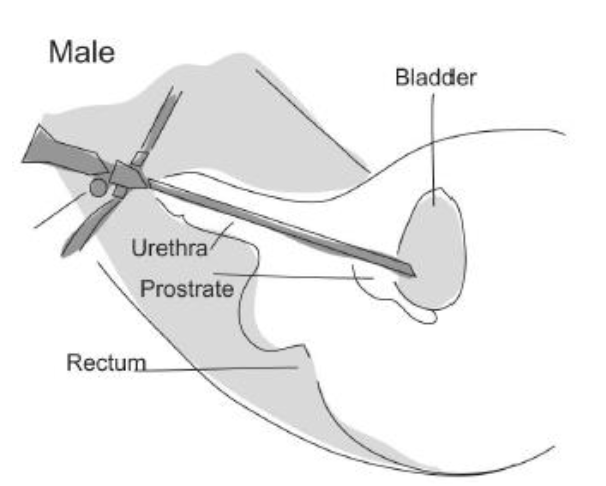
Cystoscopy is a procedure that allows the inside of the bladder to be inspected with a telescope. Cystoscopy also allows access to the ureters, which are the tubes that allow urine to drain into the bladder from the kidneys. When used to view the ureters, this called a ureteroscope.
What is urethroscopy?
Urethroscopy is a procedure that allows the inspection of the urethra (water pipe) with a telescope.
Why do I need a cystoscopy and/or a urethroscopy?
Both cystoscopy and urethroscopy are performed to diagnose and treat disorders of the bladder and urethra. Your hospital doctor may recommend either of these procedures for any of the following conditions or symptoms:
- Frequent urinary tract infections.
- Blood in your urine (haematuria).
- Loss of bladder control (incontinence) or overactive bladder.
- Unusual cells found in urine sample.
- The need for a catheter to be inserted into the bladder.
- Painful urination, chronic pelvic pain or interstitial cystitis.
- Urinary blockage such as prostate enlargement, stricture or narrowing of the urinary tract.
- Stone in the urinary tract.
- Unusual growth, polyp, tumour or cancer.
What is a flexible cystoscopy?
A ‘flexible’ cystoscopy is a cystoscope with a special flexible telescope that is usually performed under a local anaesthetic, whereby anaesthetic gel is inserted into the urethra (water pipe) before the telescope is inserted. This is an investigation (a look); no cutting will take place during this procedure.
What is a rigid cystoscopy or urethroscopy?
A rigid cystoscopy or urethroscopy is performed under general anaesthetic (while you are asleep). This allows a biopsy (tissue sample) of the bladder to be taken if required.
What is a check cystoscopy?
A check cystoscopy is a repeat examination of the bladder under a general anaesthetic, following a diagnosis of bladder cancer. This is to assess for the re-growth of tumours.
Alternative investigations
Investigations such as an X-ray, scans, urine tests and an external examination may help to identify the cause of a urinary symptom. However, they do not provide enough information so cannot replace cystoscopy, which is a direct way of examining and, in some situations, treating a problem in a single procedure.
Possible risks
Infection
Introducing anything into the bladder carries the risk of infection, no matter how sterile the procedure. Signs of infection are frequency, urgency and severe burning when passing urine. A temperature may accompany these symptoms and some patients experience a bearing down sensation. You may feel the need to pass urine, even when there is no urine in your bladder. If infection happens during your stay in hospital, you will be treated with antibiotics.
If all or some of these symptoms continue or develop after you have been discharged, please contact your GP urgently.
Please note that you may find that it is quite sore and/or painful when you pass urine and you may experience some frequency and urgency of passing urine following the procedure. These symptoms are common and normal. However, if the symptoms do not settle after 24 to 48 hours, please contact your GP for advice.
Perforation
If biopsies or cauterisation of tissue is performed, there is a small risk that a hole may develop in the bladder and urine could leak into the pelvis. If this happens a catheter will be placed into the bladder. The catheter will be left inside the bladder to allow time for the hole to heal. You may be discharged with the catheter in place.
Haemorrhage
If any biopsies have been taken, there is a small risk of bleeding. If this happens, any fluid lost will be replaced via a drip; a thin tube inserted into your arm. Very rarely, a blood transfusion may be necessary.
Pre-assessment
You will be assessed for a rigid cystoscopy or urethroscopy either in the Pre-admission Clinic, or by telephone, for suitability to have the procedure.
The procedure may be done as a day case, or as an inpatient, depending on your general health or on the expected outcome of the surgery. You will be given instructions about diet and what to bring into hospital. You will also be given the opportunity to ask any questions that you may have.
This is not required for a flexible cystoscopy as this is performed under local anaesthetic.
Before the operation
Do not eat or drink for 6 hours before your operation. You will usually be advised on what time to stop eating and drinking at the Pre-admission Clinic.
If you are having a local anaesthetic, you may not have to starve.
An anaesthetist will see you before your operation to assess your fitness for anaesthetic and to discuss, with you, the methods available. While taking your preference into account, as well as any medical conditions you may have, the anaesthetist will make the final decision based on the method of anaesthetic that is safest for you.
Discharge
Please arrange for somebody to drive you home from hospital. You should not drive after receiving a general anaesthetic. You will also need an adult to be with you for the 24 hours following your surgery. If this is not possible, please let the nursing staff know as they may wish to arrange for a district nurse to visit if necessary.
Contact information
If you have any concerns during the 48 hours following your surgery, please contact the nursing staff in the departments listed below. After this period, please contact your GP for advice.
Urology patients:
Your Consultant’s Secretary
Tel: 0300 422 6902 - select Option 1
Monday to Friday, 9:00am to 4:00pm
Urology Nurse Practitioners
Tel: 0300 422 6902 - select Option 3
Monday to Friday, 9:00am to 4:00pm
Chedworth Day Unit
Tel: 0300 422 3399
Monday to Friday, 9:00am to 8:00pm
Gynaecology patients:
Urogynaecology Team
Tel: 0300 422 6278
Monday to Friday, 9:00am to 4:00pm
Gynaecology Outpatients
Tel: 0300 422 6248
Monday to Friday, 9:00am to 5:00pm