Procalcitonin (PCT)
Chemical Pathology
Notes
Please note that this test is not routinely available except for the department of critical care.
Any other requests should first be discussed with a Critical Care Consultant or with a Consultant Microbiologist.
Procalcitonin (PCT) is the precursor of the hormone calcitonin, which in normal metabolic conditions is mainly produced by the C‐cells of the thyroid medulla and to a lesser extent by other neuroendocrine cells. The blood of healthy individuals contains only very low levels of PCT.
Following pro-inflammatory stimulation (particularly systemic bacterial infection), PCT is produced by numerous cell types. PCT affects the immune response by modulating the induction of pro-inflammatory cytokines. It also acts as a chemokine, influencing the migration of monocytes and parenchymal cells to the site of inflammation. PCT plays a role in vascular contraction through inhibiting or activating the induction of inducible NO‐synthase.
Increased PCT levels are therefore found in patients suffering from bacterial sepsis, especially severe sepsis and septic shock. PCT has been proposed as a tool to guide decisions relating to antibiotic requirements. As a biomarker of infection it has many ideal properties including a rapid rise in response to stimulation and a fall in response to control of the infection.
NICE Diagnostic guidance DG18 (October 2015) does not currently support routine use of PCT in the NHS due to insufficient evidence; however in the GHNHSFT Critical Care Departments only, PCT is being used to guide discontinuation of antimicrobials as this is where the evidence is strongest.
Sample requirements
- If patient on high dose biotin therapy (>5mg/day) collect sample at least 8 hours after the last dose
- Requests for procalcitonin always require a fresh sample. The test cannot be added to a sample already in the laboratory because of the risk of carryover.
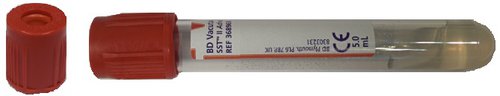
For adults, 3.5 ml of blood taken into a rust top gel tube.
Storage/transport
Send immediately to the laboratory at room temperature. Samples need to be centrifuged within 4 hours.
Required information
Relevant clinical details including reason for the request.
Turnaround times
The assays are run at the Gloucester laboratory during the day (9am to 5pm), Monday to Friday only with results normally available within 1 hour of sample receipt in the Gloucester laboratory.
Reference ranges
Expected values
Normal range: <0.05ng/mL
Clinical cut-off:
<0.50ng/mL represents a low risk of severe sepsis and/or septic shock
>2.00ng/mL represents a high risk of severe sepsis and/or septic shock
PCT is normally less than 0.05 ng/ml (equivalent to less than 0.05 ug/L) in healthy individuals. note however that normal levels do not exclude infection. All results should be interpreted in the context of the patient's clinical history.
Local treatment guidelines
- PCT is not a substitute for good clinical judgement and cannot be used in isolation.
- PCT <0.5 ng/ml – minimal PCT response. Ongoing infection unlikely therefore witholding antimicrobials strongly advised.
- If PCT was also measured at the start of treatment a fall by more than 90% from this initial value suggests antimicrobials can also be stopped. If this initial value was <0.5ng/ml non-bacterial infections or causes of systemic inflammation should be considered.
- PCT >0.5 ng/ml – continue antibiotics
- If follow-up PCTs fail to fall then this suggests either treatment failure or a new source of infection. Appropriate investigations should be performed (e.g. full septic screen, imaging) and a change in antimicrobial therapy considered.
- PCT may be elevated in any condition where a significant systemic inflammatory response is seen, e.g. following major trauma, surgery, burns, pancreatitis.
- A PCT of < 4ng/ml in patients with acute pancreatitis (within 48h of onset) suggest bacterial infection is unlikely.
- PCT may be falsely elevated in small cell lung cancer or medullary C-cell carcinoma of the thyroid.
Further information
Monograph of the Association for Clinical Biochemistry and Laboratory Medicine