Gloucestershire home enteral feeding team (HEFT)
The home enteral feeding team (HEFT) provide a countywide service to patients in Gloucestershire. Find out what we do, meet the team, and check how to make referrals.
On this page
-
What is enteral feeding
-
Our Team
-
Who is the service for?
-
What we do
-
Where do I get my tube feed and equipment?
-
What can our team help with?
-
Training in the community
-
What happens at discharge from hospital?
-
Collaborative work
-
What happens if I need to go into hospital with my feeding tube?
-
Neurology clinic
-
Contact us
-
Useful Links and Videos
What is enteral feeding
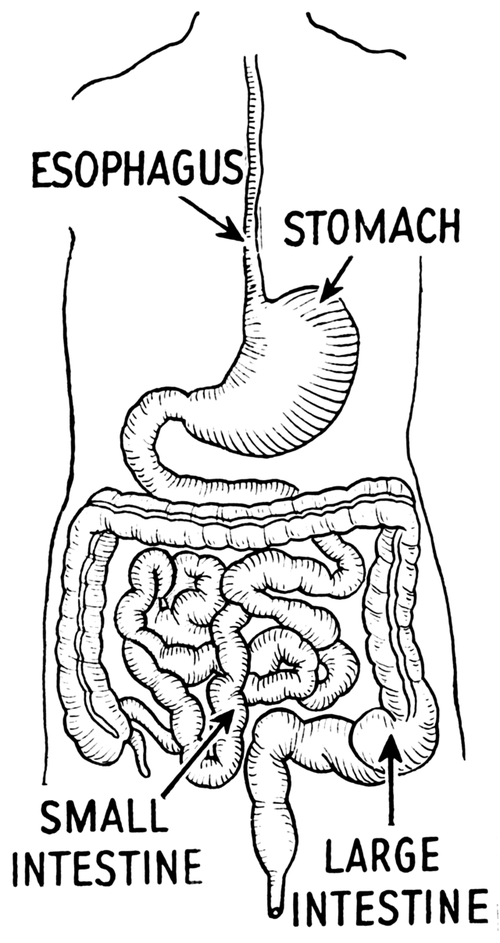
If you're finding it difficult to eat or drink enough to get the nutrients your body needs, your healthcare team might recommend a liquid diet delivered directly into your stomach or small intestine. This is called enteral feeding.
How Does It Work?
Short-Term Feeding
- A soft tube, called a nasogastric (NG) tube, is gently inserted through your nose and down into your stomach.
- Liquid food is then passed through this tube. This liquid contains all the nutrients your body needs.
- Depending on your needs, the feed might be given slowly over a few hours or in smaller amounts at set times, like meals.
- If your stomach isn't working properly, a similar tube called a nasojejunal (NJ) tube will be placed further down into your small intestine (jejunum).
These tubes are usually for short-term use.
Long-Term Feeding
- If you need tube feeding for more than 4 weeks, a different type of tube might be used. These include:
- A gastrostomy or PEG tube (placed directly into your stomach through your abdomen).
- A jejunostomy tube (placed directly into your small intestine).
The PEG tube is usually placed using a procedure called an endoscopy. In some cases, it may be done surgically or with X-ray guidance. The jejunostomy tube is placed surgically.
Support and Care
Your healthcare team will provide everything you need to make tube feeding as simple and safe as possible. They'll also create a care plan tailored to you, which will include:
- How much feed you need and when to take it.
- How they will monitor your health.
- How to use and care for your equipment.
- Arrangements for regular deliveries of supplies and who to contact for help.
- Guidance on common problems and how to solve them.
- Emergency contact numbers and a helpline for questions.
Your healthcare team will also make sure you and your carers get the right training and support to feel confident managing tube feeding.
Our Team
The Gloucestershire Home Enteral Feeding Team (HEFT) is based at Gloucestershire Royal Hospital under the Nutrition and Dietetic Department. We provide countywide support to children and adults with enteral feeding tubes in the community. Our team is made up of:
- Specialist Dietitians
- Enteral Nutrition Nurse Specialists
- Dietetic Assistant Practitioners and Dietetic Support Workers
- Administrative Staff
Our dietitians are all registered and regulated by the Health & Care Professions Council and our nutrition nurses are all registered and regulated by the Nursing & Midwifery Council.
Who is the service for?
Most adults and children who have enteral feeding tubes and are registered with a Gloucestershire GP are looked after by the Gloucestershire HEF team. If you have been discharged from a local hospital with an enteral feeding tube, our team should receive a referral from your hospital dietitian. If you are moving into the area, please request your previous HEF dietitian contact us to transfer your care.
What we do
Our team works closely with the local community to support patients with enteral feeding tubes at home or in specialist centres. We visit a variety of community settings including:
- patients’ homes
- respite centres
- schools
- care homes
- patients’ place of work
Our dietitians will create a feeding plan which works for you and will monitor your nutritional intake to support your health. Your dietitian may also be able to help with your tube and stoma site care, or will liaise with our specialist nurses.
Our Enteral Nutrition Nurse Specialist team provide support and advice on enteral feeding tubes, enteral feeding equipment, stoma sites, and medication administration via enteral feeding tubes.
Our Dietetic Assistant Practitioners and Support Workers collect relevant medical, social and dietary information from the patient, carer, medical, nursing and other healthcare staff and feedback to the registered clinicians. They undertake measurements such as weight and height, assist with ordering patient enteral feeding supplies, assess enteral feeding tubes/stoma sites and undertake basic tube care to support the wider team.
Our administrative staff maintain a front-line administrative service and thereby support the rest of the team.
Where do I get my tube feed and equipment?
Our team currently have a contract with a feeding supplies company called Nutricia. You will be registered on their system Nutricia Homeward by your dietitian to receive monthly home deliveries of the following items (as required):
- 60ml purple enteral syringes (single-use or reusable as appropriate)
- Feed (small bolus bottles or larger pump bottles)
- A Nutricia feeding pump, stand and pump-giving sets
- Sterile containers (to pour feed or water into)
- Bolus adaptors (to enable a syringe to connect to the larger pump bottles of feed)
- 5ml syringes and pH paper (for checking the position of a balloon gastrostomy tube, button tube or nasogastric tube)
- Spare feeding tube and accessories
Nutricia Homeward deliveries will be arranged on your behalf before discharge.
We do advise that you keep a 7-day buffer stock of all required items as well as your monthly supplies. This is important to avoid under or over-stocking of supplies which can lead to shortage or wastage. Please note that emergency stock orders can take up to 2 working days to arrange. You can manage your monthly stock checks online by ordering here.
You can contact Nutricia for supply and delivery issues either during office hours (Monday to Friday 9am-5pm) on 0800 028 2667 (free from a landline) or out of hours (Monday to Friday after 5pm) on 0800 093 3672. If you have any feeding pump issues outside our team’s working hours, please contact the Nutricia out of hours helpline.
Please remember to keep all medical supplies out of reach of children and vulnerable adults.
Other supplies
There are some supplies that our team are not able to provide including syringes for medication, ampoules of water for injection, dressings or tape. Some items require a GP prescription, so our team will request these via your GP surgery.
What can our team help with?
- Providing support and monitoring of your feeding/fluid needs including any practical feeding concerns, weight concerns, tolerance concerns, (e.g., vomiting, diarrhoea, constipation.), getting copies of your feeding/fluid plan and if you have a problem with your feeding pump
- Providing training to set up your feed and equipment
- Providing advice on looking after your feeding tube and stoma site
- Liaising with Nutricia if you have any delivery issues
- If you are planning a holiday and need a letter or supplies to be organised from Nutricia (please request this as soon as you have planned your holiday)
- Support with any emotional and social aspects of enteral feeding
Training in the community
Our Enteral Nutrition Nurse Specialists offer Bespoke Gastrostomy Training to community care providers via a face-to-face training package.
Session details:
The session will cover general principles of enteral feeding tube care and troubleshooting
- The session will be tailored to suit you and your client/service user, covering their specific tube types and feed methods.
- The session will be between 1.5 – 3 hours long depending on need and priced between £534.95 and £600.45.
- Maximum of 12 people per session.
- Knowledge assessment on completion of the training.
- The care provider is responsible for booking an appropriate training room with adequate space for practical demonstration.
- Sessions are currently offered Mondays and Thursdays, 10am – 12pm or 1 - 3pm.
Please request that any care providers who will be taking over patients’ tube care on discharge and are new to (or require refreshers on) gastrostomy management contact our team for further details including cost.
Interested in training? Register here
What happens at discharge from hospital?
Each patient requires different items depending on their dietetic care needs and feeding tube type.
On discharge from a Gloucestershire Royal Hospital / Cheltenham General Hospital ward, you should be provided with:
- At least 7 days’ supply of purple enteral syringes. Please note that some enteral syringes are single-use while others are reusable
- If you have been provided with a stoma stopper, please bring this with you
- At least 7 days’ supply of sterile gauze and sterile saline (if the tube has been in for less than 14 days on discharge)
- A Nutricia pump, stand and 7 days’ supply of pump giving sets (if required)
- At least 7 days’ supply of feed (if required)
- A spare balloon gastrostomy tube (if required)
You should also receive the following from the ward dietitian:
- A discharge information pack
- Feeding/fluid plan
Going home with a new enteral feeding tube can be overwhelming. After discharge from the hospital, you should receive a phone call from a member of the HEF Team. This will be to arrange a suitable date for a dietitian and/or enteral nutrition nurse specialist to visit you at home, as well as discuss any concerns you may have at the time.
The purpose of our home visit is to discuss and provide support and advice regarding your dietetic care needs, feeding tube and stoma site. As long as you remain under the service, you will be contacted regarding follow-up visits. Routinely these take place every 6 months, but this may vary depending on team capacity and clinical need. Support between visits will be available via telephone and email (see our contact details below).
Home visits
By agreeing to be seen by the HEF team we will assume that you are consenting to treatment from us. We will always discuss any treatment with you and agree on an appropriate treatment plan to best suit your needs.
Things we may monitor and discuss with you:
- weight and height (sometimes we may also take additional measurements such as head circumference in babies, waist circumference, handgrip strength, or skinfold measurements)
- your nutrition and fluid plan (we will ensure you are provided with a written/digital copy of this)
- your bowel and urine habits
- any lifestyle changes
- any recent blood results
- your tube and feeding equipment
- your stoma site (skin surrounding your tube). To help us monitor any treatment it may also be useful for us to take a photograph of your stoma site. We will ask for your consent before doing this.
Our expectations during all home visits:
- Please do not smoke in the room where the review is taking place
- Please remove pets from the room where the review is taking place
- Please treat all members of the HEFT with kindness and respect
First home visits may last between 60 - 90 minutes. Future visits will usually be shorter.
Please note that we may need to rearrange your appointment at short notice if necessary.
Collaborative work
If you are referred to a consultant out-of-area but remain registered with a Gloucestershire GP, your dietetic care needs and enteral feeding tube may be managed under the shared care of our team and your out-of-area dietitians / nutrition nurses. Please inform us if there are any changes advised by your out-of-area team, so we can make adjustments to your feeds and/or equipment orders.
The HEFT liaises closely with other professionals (such as GP’s, consultants, community nurses, speech and language therapists, etc). Information gathered during your consultation may be sent as a letter update to you and relevant healthcare professionals involved in your care. Please inform us if you do not wish for your information to be shared with other healthcare professionals.
What happens if I need to go into hospital with my feeding tube?
If possible, please contact our team if you have been admitted to the hospital so that we can ensure a handover is done to the hospital dietitian. Please take the following supplies to the hospital:
- If you have a balloon gastrostomy tube or button, please bring the spare tube/button and extension sets with you. These will not be supplied by the hospital
- If you have a PEG, please bring your spare Y adaptor repair kits or Freka repair kit
- A copy of your most up-to-date feeding/fluid plan
You do not need to bring your feeding pump or feed unless you are asked by the HEFT or ward dietitian.
Please be aware that patients have different tubes and therefore some of the items listed above may not be relevant.
Neurology clinic
The neurology clinic is run by the HEF team’s neurology dietitian. It takes place in the afternoon at the Gloucester Royal Hospital outpatient department on the 2nd and 4th Wednesdays of the month. Patients who are referred to this clinic will be required to have a diagnosed neurological condition. Types of conditions that are covered by the clinic include:
- Motor Neurone Disease (MND)
- Multiple Sclerosis (MS)
- Parkinson’s Disease
- Progressive Supranuclear Palsy (PSP)
- Multi-System Atrophy (MSA)
- Huntington’s Disease
- Brain Injury
- Brain tumour (those not or no longer undergoing oncology treatment, as these patients may fall under the oncology Dietetic service)
- Gillian Barre Syndrome (GBS)
- Spinal Injury
- Muscular Atrophy/Muscular Dystrophy
- Human variant CJD
The neurology dietitian will complete a nutrition assessment, including weight monitoring (as possible) to determine the patient’s nutritional status and nutritional intake. They will then offer advice on food and drink fortification, Oral Nutritional Supplements (ONS) and further enteral nutrition support as required.
Please note that patients must be able to attend the clinic appointment to be eligible. We are unfortunately unable to undertake consultations via the telephone.
Referrals are accepted from the following sources:
- Consultants
- GP’s
- Neurology Specialist Nurses
- The Brain Injury Team
- Speech and Language Therapists
- Dietitians
Referrals can be accepted from across the county of Gloucestershire, provided the patient's GP is included within the list of Gloucestershire GPs.
GPs can refer to this clinic via ERS (electronic referral system).
Gloucestershire Hospitals NHS Foundation Trust / Gloucestershire Health and Care staff, incl. Consultants and Specialist Neurology Nurses can refer neurology patients to this clinic via a letter to the HEF team.
Contact us
Please contact us if you feel that you need to be seen sooner than your next scheduled appointment. Please also contact us if there are any problems or changes relating to your feed, your feeding tube or stoma site, or if you have been admitted to the hospital.
If you are a healthcare professional and need to refer a patient to our services, please contact us for a referral form.
You can email us at ghn-tr.homeenteralfeedingteam@nhs.net or call us on 0300 422 5645. Please be aware that email is not a secure means of communication. If you require a secure means of communication or need to speak to someone urgently, please contact us by telephone. Unfortunately, we may not always be able to answer our phone lines, but voicemail messages and emails are checked regularly during office hours and someone will get back to you as soon as possible.
Please note we are not an emergency service. Our office hours are Mon-Fri 8.30am to 4.30pm excluding bank holidays. If a patient requires any urgent feed or tube related advice outside of these hours, please refer them to their out of hours GP, district nurses (adult community nursing team), CCN’s (children’s community nursing team), PAU or NHS 111.
If your query is not related to your feed or feeding tube, we may not be the best-placed professionals to help. In this instance, your GP, NHS 111 or in an emergency 999 may be more appropriate.
Useful Links and Videos
- VIDEO – How to Replace a CORFLO PEG Y adaptor and perform Advance and Rotate
- VIDEO – How to Replace a FREKA PEG connector and perform Advance and Rotate
- VIDEO – How to check the volume of a balloon Gastrostomy Tube
- VIDEO – How to replace a balloon Gastrostomy Tube
- VIDEO – Taking a Mid-Upper Arm Circumference (MUAC)
PINNT Support Group – PINNT (Patients on Intravenous and Naso-gastric Nutrition Treatment) is a charity providing support for people on home enteral feeding
Carers UK - provides information and advice on caring, helps carers connect with each other, campaign with carers for lasting change, and use innovation to improve services.
Discharge advice following a gastrostomy tube removal
Daycase Percutaneous Endoscopic Gastrostomy (PEG) Tube procedure
Administering Medications via Enteral Feeding Tubes